Preventing Heart Attacks Before They Happen: How AI Is Transforming Healthcare
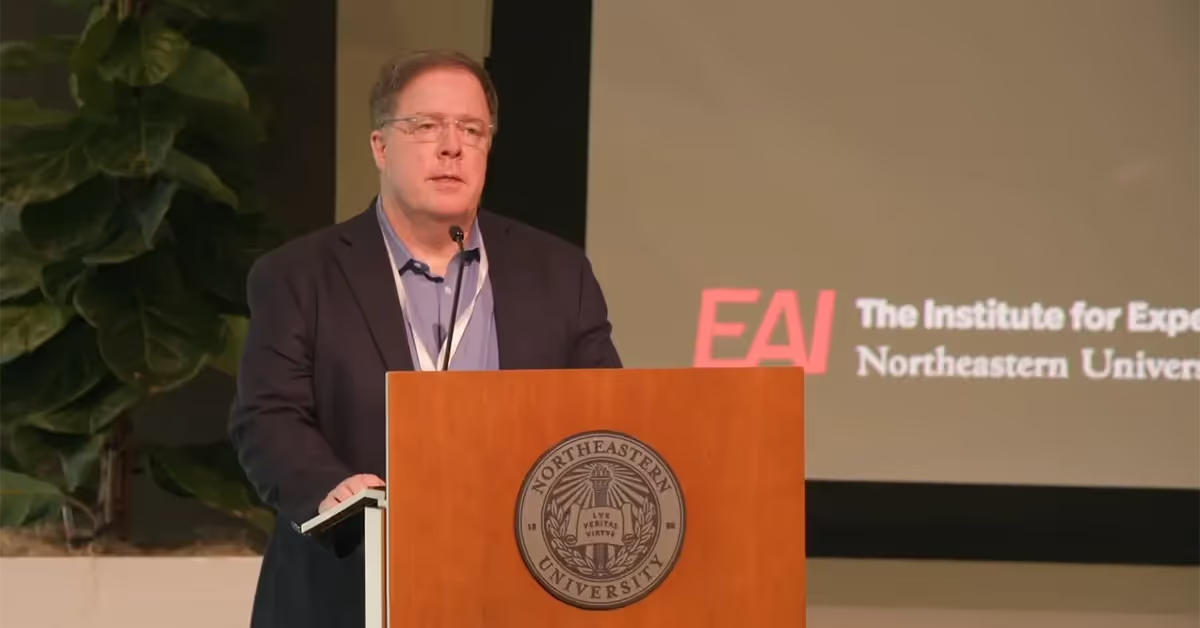
Imagine a healthcare system where clinicians can anticipate when their patient is about to have a heart attack and prevent it before it unfolds. That was the bold vision laid out by Timothy Ruchti, the director of algorithms at Nihon Kohden Digital Health Solutions, at The State of AI in Precision Health conference hosted by the Institute for Experiential AI at Northeastern University Oct. 10.
Ruchti’s presentation offered a compelling vision for the future of healthcare powered by artificial intelligence. His presentation focused on AI's ability to predict clinical events using continuous monitoring data – a capability he believes will become the norm.
“I firmly believe that this is going to be standard of practice in the future because there are benefits to the clinician, significant benefits to the patient, and there is data that has not been tapped to its full potential,” Ruchti told a packed audience on the 17th floor of Northeastern University’s East Village.
For healthcare executives trying to tap into AI-driven innovation, Ruchti’s insights provide a roadmap for using advanced predictive analytics to change the way they care for patients.
“Our value proposition is, let’s inform clinicians early so they can make proactive decisions about treatment and thereby reduce the number of adverse clinical events and improve outcomes,” Ruchti said.

AI For Predictive Health Modeling
Healthcare providers today face a significant challenge: Monitoring multiple patients continuously while detecting subtle signs of deterioration before they become critical. While experienced clinicians can often identify deteriorating patients, they can't monitor all patients at all times. That’s where AI comes in.
Ruchti discussed the use of cardiorespiratory devices for real-time health monitoring, highlighting AI's ability to detect subtle physiological changes in the data — signals often undetectable by clinicians due to the sheer volume of data and time constraints.
With the ability to alert clinicians to early-stage deterioration, these models enable proactive interventions, improving patient outcomes and potentially reducing mortality rates associated with acute events like heart attacks.
Ruchti highlighted several key advantages of combining continuous bedside monitoring with AI:
- Automatic data collection requires no additional tests
- Continuous measurements enables real-time model updates
- Objective physiological indicators are free from clinical bias
- Rich information density (e.g., 13,000 continuous heart rate measurements versus four manual heart readings over the same period)
One example Ruchti discussed is a model for predicting cardiac arrest using photoplethysmography (PPG) data. Developed by a researcher at Emory University, the model was trained on six million hours of data to predict the likelihood of cardiac events.
The results underscore a generalizable finding across AI research: larger datasets and model complexity correlate with better performance.
Advice for Healthcare Leaders
Ruchti says healthcare executives need to integrate predictive AI models into routine clinical workflows to maximize their value. Developing models in collaboration with clinical stakeholders also ensures they address real-world needs and are usable in everyday practice.
“It’s important that model development begin and end in the clinic,” Pick a solution that is important to the clinician and then during development consider how that solution is going to be integrated into the clinical setting.
Ruchti noted that Institute for Experiential AI Affiliate Faculty Rai Winslow, who is also Director of Life Science and Medical Research at the Roux Institute, has been following that approach as part of a collaboration with MaineHealth and Nihon Kohden. That works because engaging with clinicians helps identify the most important problems worth solving.
A central example of predictive technology in action is CoMET, Nihon Kohden’s emergent intubation model. Deployed in clinical settings, CoMET alerts healthcare providers to a patient's increased risk of intubation hours before it might become necessary. Such lead time can allow for preventive measures, improving patient stability and care.

Partnerships Designed For Impact
Ruchti’s presentation showed predictive modeling holds enormous promise for improving patient outcomes, optimizing clinical resources, and creating a new standard of care. But realizing this potential will require careful consideration of model development, clinical integration, and operational deployment as part of a larger care ecosystem.
The Institute for Experiential AI partners with healthcare organizations to help them tap into the power of AI through a series of tailored offerings. We can identify the highest ROI opportunities for AI based on your data, offer independent “AI Advisory Boards” made up of industry veterans, and build custom AI solutions that future-proof your organization.
Learn more about our AI solutions for health and life sciences partners.
Watch Ruchti’s talk below and explore more coverage from The State of AI in Precision Health!